- Ved WFsensorer
Clinical and surgical monitoring demand continuous, low-latency, traceable blood pressure signals. Accurate readings matter — drug dosing, blood-flow management and ECMO settings all rely on real-time pressure traces. Typical healthy references sit around 90/60 to 120/80 mmHg, but critically ill patients and certain therapies (for instance, ECMO) need a wider monitoring capability and faster response. To cover these cases, sensors should support high sampling rates, low-noise amplification, an appropriate measurement span (for example, -30 to 300 mmHg or wider) and good biocompatibility and structural strength.
Katalog
1. Design principles and core modules
To nail clinical-grade accuracy you must optimise the full signal path — from diaphragm and bridge through to system-level electronics and packaging.
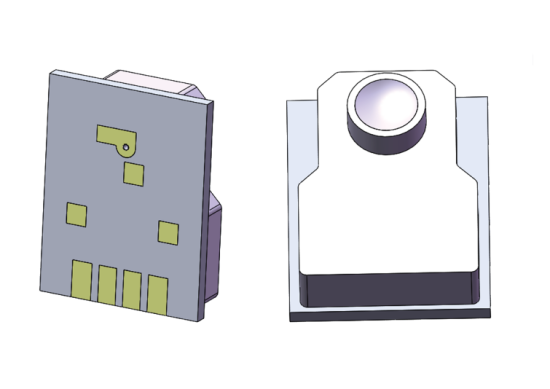
Sensing element. A silicon piezoresistive MEMS structure gives the quick response you need to capture arterial waveforms with the required bandwidth and linearity. When you design the element, prioritise low non-linearity, minimal hysteresis and fast recovery so the sensor still catches peaks and pulses during rapid heart rates or sudden pressure swings.
Packaging and media interface. Invasive setups put blood or catheter fluid in contact with the package, so the enclosure must minimise contact volume to lower clotting risk. Small-diameter seals and medical-grade dielectric gels help reduce blood contact without losing sensitivity.
Signal conditioning. The front-end amplifier should have high input impedance, low drift and use passive temperature-compensation strategies where possible. Pair that with an anti-aliasing filter that preserves the 0–40 Hz blood-pressure band while rejecting mains and EMI. A digital back end with stored calibration parameters makes it easy to linearise output and apply corrections.
System robustness. Build the device to withstand burst pressures and fatigue over time. Choose materials and mechanical designs that don’t fail under extreme pressure events.
Sensor module breakdown and implementation focus
Treat the sensor as four subsystems: sensing element, media-isolation, front-end amplifier and digital calibration. Test each block to clinical-grade standards: zero stability, sensitivity drift, linearity error, shock and vibration response, and long-term behaviour in biological fluids. For the front-end, use low-noise op-amps and a differential bridge to boost SNR; carefully route the PCB to avoid parasitic capacitance and unwanted mechanical coupling introduced by soft tubing. Make sure the front-end retains linearity and stability when exposed to routine static pressures up to 300 mmHg and transient pressure spikes.
2. Pressure-range selection and span strategies
Clinical use ranges from standard bedside monitoring to surgical and ECMO environments — each has different span and surge requirements. Picking the right range affects not only measurement accuracy but also device lifetime and cost.
Span recommendations. For invasive arterial lines, a -30 to 300 mmHg range covers most scenarios; offer an extended option for -500 to 1000 mmHg when needed. The extended span must still provide a calibratable linear output and traceable error bounds across the full interval. Pumps and pressure bags used in clinical set-ups often push to 300 mmHg to manage flow and avoid backflow, so the sensor must tolerate that static load without degradation.
Temperature and environment. Medical devices usually operate between about 15–40°C. Prefer sensors with good passive compensation across that band, which simplifies calibration and improves field usability. Some sensor variants include an integrated temperature sensor to enable software compensation.
Range validation and clinical matching
Range validation should include two test families: static linearity and accuracy over the full range (0–300 mmHg or the extended interval), and dynamic-response testing (step, pulse and frequency response). Temperature compensation may be passive at the component level or implemented digitally using direct temperature readings; the latter offers finer control and easier multi-point correction. For high-dependability applications like ECMO, add wet-heat cycles and long-term soak tests in validation to mimic actual use conditions.
3. Biocompatibility, packaging and media management
Anything that touches blood or sits in the fluid path needs special consideration. The goal is to minimise blood contact volume, cut down clot and deposit risk, and allow straightforward sterilisation or single-use strategies.
Packaging points. Use small-diameter seals to reduce exposed blood volume and medical-grade dielectric gels as a media barrier — these provide electrical insulation and mechanical coupling while being straightforward to validate for compatibility. Smaller seals reduce local blood retention, lessening the odds of thrombus or fibrin build-up — both of which would corrupt readings over time.
For reusable parts, design the flow path to be easy to flush and disinfect; for disposables, pick materials and sealing approaches that favour low cost and manufacturability.
Packaging details and blood compatibility
Choice of seal diameter (standard 4.8 mm or a smaller 3.2 mm, for example) directly affects device footprint and exposure risk. Materials must pass biocompatibility checks, and the design should be prototyped and tested in flow rigs that reproduce pulsatile blood flow to confirm there’s no local low-flow region that would cause deposition. Quick media-compatibility checks during development shorten the prototype cycle.
4. Compliance, testing and long-term reliability
A medical-grade pressure sensor must meet industry standards and regulatory requirements covering performance, materials and safety. Conformance isn’t just for market entry — it builds clinical trust.
Key standards. There are specific test standards for blood-pressure sensor performance and safety. Validate burst pressure, sensitivity stability, temperature drift and long-term drift with accelerated life testing. Manufacturing tests should include full-range calibration across 0–300 mmHg and batch sampling.
Lifetime and warranty. Clear warranty terms (for example, a three-year product life claim) help clinical buyers plan maintenance. Define separate acceptance and end-of-life checks for disposables and reusables so final assemblies match documented specs.
Performance validation workflow and compliance paperwork
Your V&V plan must include static accuracy, dynamic response, burst and fatigue testing, temperature cycling and biological fluid soak tests. Compile complete technical documentation to back up compliance claims: test reports, material declarations and factory inspection logs. For devices aimed at intensive care and ECMO, add higher-reliability analysis and a focused FMEA exercise.
5. System integration, footprint optimisation and field calibration
When you integrate the sensor, coordinate the mechanical, electrical and software aspects so the final device is usable and maintainable at the bedside.
Size and connections. An ultra-compact sensor reduces overall device footprint and eases tubing routing. Small pads or standard plug connectors speed up manufacturing and servicing; include removable electrical contacts that retain calibration data where possible. Smaller blood-contact areas also lower disposable costs and improve safety.
Field calibration and diagnostics. Provide a simple, reliable zeroing routine that clinical staff can run on installation. Integrate self-test features and alarm thresholds to flag pressure deviations or line occlusions early.
Integration strategy and maintenance concerns
At system level, arrange PCBs and the sensor to minimise flow-path length and thermal coupling. Use software to implement progressive compensation over time and temperature. Ultra-compact solutions win in portability and emergency use, but you must demonstrate no performance loss under shock, vibration and pulse loading during reliability testing.
Konklusjon
Creating accurate blood pressure sensors for medical devices requires striking a balance between sensitive components, packaging, signal conditioning, range selection, compliance testing, and system integration. For clinical scenarios (especially ECMO and intensive care), it is recommended to prioritize validated designs ranging from -30 to 300 mmHg, or, if necessary, extended range versions. Ultra-compact sensors that reduce blood contact volume should be selected to minimize the risk of clotting and improve long-term stability. The manufacturing and validation process should include comprehensive temperature, dynamic response, and biocompatibility testing, and technical documentation and test reports supporting compliance claims should be prepared. The engineering considerations and validation steps outlined in this article provide R&D teams with an actionable roadmap to help quickly and safely advance designs to clinical deployment.
Introduksjonen ovenfor skraper bare overflaten av applikasjonene til trykksensorteknologi. Vi vil fortsette å utforske de ulike typene sensorelementer som brukes i ulike produkter, hvordan de fungerer, og deres fordeler og ulemper. Hvis du vil ha mer detaljer om hva som er diskutert her, kan du sjekke det relaterte innholdet senere i denne veiledningen. Hvis du er presset på tid, kan du også klikke her for å laste ned detaljene i denne veiledningen Lufttrykkssensorprodukt PDF -data.
For mer informasjon om andre sensorteknologier, vennligst Besøk Sensors -siden vår.
